Retinal detachment is a serious condition that can lead to permanent vision loss if not treated promptly and effectively. Understanding the causes, symptoms, and treatment options is crucial to preserving your vision. In this article, we will explore the different types of retinal detachment treatment options, post-treatment care and recovery, and preventive measures you can take.
Understanding Retinal Detachment
Retinal detachment is a serious condition that occurs when the thin layer of tissue at the back of the eye, known as the retina, separates from its underlying supportive structures. This separation can disrupt the blood supply to the retina and lead to vision loss.
Retinal detachment can be caused by various factors, including:
- Trauma: A direct injury to the eye can cause the retina to detach. This can happen due to accidents, sports injuries, or any other impact to the eye. The force exerted on the eye can cause the delicate retina to tear away from its supportive tissues, leading to detachment.
- Age: Retinal detachment is more common in individuals over 40 years old. As we age, the vitreous gel inside our eyes can shrink and become more liquid, increasing the risk of the retina detaching.
- Previous Eye Surgery: Certain eye surgeries, such as cataract surgery or laser eye surgery, can increase the risk of retinal detachment. This is because these procedures may cause changes in the structure of the eye, making the retina more susceptible to detachment.
Causes of Retinal Detachment
One of the most common causes of retinal detachment is a tear or hole in the retina. When a tear or hole occurs, it allows fluid to accumulate between the retina and its supporting layers, causing detachment. Other causes of retinal detachment include:
- Vitreous shrinkage and detachment: As mentioned earlier, the vitreous gel inside the eye can shrink and become more liquid with age. When this happens, it can pull away from the retina, causing it to detach.
- Tumors affecting the retina: In rare cases, tumors can develop on or near the retina, leading to retinal detachment. These tumors can put pressure on the retina or its supporting structures, causing them to separate.
- Genetic predisposition: Some individuals may have a genetic predisposition to retinal detachment. Certain genetic factors can make the retina more prone to tearing or detachment, increasing the risk of this condition.
Symptoms and Early Warning Signs
Recognizing the early warning signs of retinal detachment is crucial for timely intervention and prevention of further damage to your vision. The symptoms may include:
- Flashing lights or sudden appearance of floaters: If you notice flashes of light or the sudden appearance of small specks or cobweb-like shapes floating in your field of vision, it could be a sign of retinal detachment. These floaters are caused by the vitreous gel pulling on the retina.
- A curtain-like shadow over the visual field: Another common symptom of retinal detachment is the presence of a shadow or curtain-like obstruction in your visual field. This occurs when the detached retina blocks the light entering the eye, causing a partial or complete loss of vision in that area.
- Blurred or distorted vision: Retinal detachment can cause your vision to become blurred or distorted. Straight lines may appear wavy or bent, and objects may appear smaller or larger than they actually are.
If you experience any of these symptoms, it is vital to seek immediate medical attention. Prompt diagnosis and treatment can help prevent further progression of retinal detachment and preserve your vision. Visit https://ighfamilyeyeclinic.com/what-to-know-about-lasik-consultation-and-some-faqs-on-its-surgery/ to read about What to Know About LASIK Consultation and Some FAQs on Its Surgery.

Different Types of Retinal Detachment
Retinal detachment is a serious condition that occurs when the retina, a thin layer of tissue at the back of the eye, becomes separated from its underlying structures. There are several types of retinal detachment, each requiring different treatment approaches:
Rhegmatogenous Retinal Detachment
Rhegmatogenous retinal detachment is the most common type and occurs when a hole or tear in the retina allows fluid to pass underneath and separate it from the underlying structures. This can happen due to trauma, aging, or other factors that cause the retina to become weak or thin. Once the retina is detached, it can no longer function properly, leading to vision loss. Immediate surgical intervention is often necessary to repair the tear and reattach the retina. During the surgery, the ophthalmologist will carefully examine the retina, identify the tear, and use various techniques to close the hole and reposition the retina back into its original position. The success of the surgery depends on the size and location of the tear, as well as the overall health of the eye.
Tractional Retinal Detachment
Tractional retinal detachment is caused by scar tissue that pulls on the retina, leading to its detachment. This type of detachment is commonly seen in patients with advanced diabetic retinopathy, a condition characterized by damage to the blood vessels in the retina due to high blood sugar levels. As the scar tissue contracts, it exerts traction on the retina, causing it to become detached. Treatment options for tractional retinal detachment may include laser therapy or surgery to remove the scar tissue and reattach the retina. Laser therapy can be used to seal leaking blood vessels and prevent further scar tissue formation, while surgery involves delicately removing the scar tissue and repositioning the retina. The success of the treatment depends on the extent of the scar tissue and the overall health of the eye.
Exudative Retinal Detachment
Exudative retinal detachment is characterized by fluid accumulation underneath the retina due to leakage from blood vessels or other abnormal sources. This type of detachment is often associated with inflammatory disorders, tumors, or choroidal neovascularization, which is the growth of abnormal blood vessels in the choroid, a layer of blood vessels beneath the retina. The abnormal blood vessels can leak fluid, causing the retina to become detached. Treatment for exudative retinal detachment usually involves addressing the underlying cause and resolving the fluid accumulation. This may include medications to reduce inflammation, radiation therapy to treat tumors, or anti-vascular endothelial growth factor (anti-VEGF) injections to inhibit the growth of abnormal blood vessels. In some cases, surgery may be necessary to drain the accumulated fluid and reattach the retina.
It is important to note that retinal detachment is a serious condition that requires prompt medical attention. If you experience sudden changes in vision, such as the appearance of floaters, flashes of light, or a curtain-like shadow across your field of vision, it is crucial to seek immediate medical care to prevent further vision loss.
Modern Treatment Options for Retinal Detachment
Retinal detachment is a serious condition that requires prompt medical attention. Fortunately, advancements in medical technology have led to various treatment options that can help restore vision and prevent further damage to the retina. Click here to read about Eye health and vision.
Pneumatic Retinopexy
Pneumatic retinopexy is a minimally invasive procedure that offers an effective way to treat retinal detachment. During this procedure, a gas bubble is injected into the eye, which helps to push the detached retina back into place. The gas bubble acts as a temporary support, allowing the retina to reattach to the underlying tissue.
In addition to the gas bubble injection, laser or cryotherapy may be used to seal the retinal tear and prevent further fluid accumulation. This combination of techniques ensures a higher success rate and reduces the risk of recurrence.
Scleral Buckling Surgery
Scleral buckling surgery is another common treatment option for retinal detachment. This procedure involves placing a silicone band, known as a scleral buckle, around the eye to provide support and relieve traction on the retina.
The scleral buckle helps to reposition the detached retina and seal any retinal tears. It acts as a permanent support, preventing future detachment and allowing the retina to heal properly. Scleral buckling surgery is often performed under local anesthesia and has a high success rate.
Vitrectomy
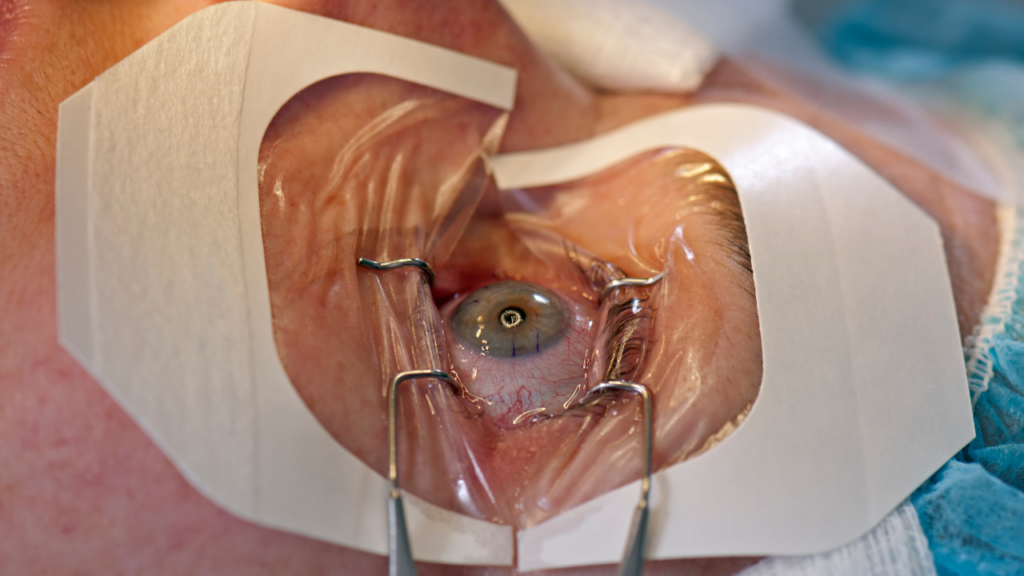
Vitrectomy is a surgical procedure that involves removing the vitreous gel, a gel-like substance that fills the eye, and replacing it with a clear solution. This allows the surgeon to access and repair the detached retina more easily.
Vitrectomy may be performed as a standalone procedure or in combination with other techniques, such as laser or cryotherapy, to ensure the best possible outcome. By removing the vitreous gel, the surgeon gains a clear view of the retina, allowing for precise repair and reattachment.
After the vitrectomy, the clear solution is injected back into the eye to restore its normal shape and function. This procedure has proven to be highly effective in treating retinal detachment, particularly in cases where the detachment is severe or complex.
It is important to note that the choice of treatment depends on various factors, including the severity and location of the detachment, as well as the overall health of the patient’s eye. A thorough examination and consultation with an ophthalmologist is crucial in determining the most appropriate treatment plan.
Overall, with the advancements in medical technology, retinal detachment can be effectively treated, allowing patients to regain their vision and prevent further complications. Early detection and prompt treatment play a vital role in achieving successful outcomes and preserving visual function.
Post-Treatment Care and Recovery
After retinal detachment surgery, it is essential to follow your doctor’s instructions for a successful recovery. Here’s what you can expect:
What to Expect After Surgery
Following retinal detachment surgery, you may experience some discomfort, redness, or blurred vision. It is normal to have a gradual improvement in vision over several days or weeks. Your surgeon will provide specific guidelines regarding activities, medications, and follow-up appointments.
Tips for a Smooth Recovery
During the recovery period, it is crucial to:
- Take prescribed medications as directed
- Avoid strenuous activities or heavy lifting
- Protect your eyes from bright lights or irritants
- Attend all scheduled follow-up appointments
Your doctor will monitor your progress and address any concerns or complications that may arise.
Preventing Retinal Detachment
While not all cases of retinal detachment can be prevented, there are steps you can take to reduce your risk:
Regular Eye Examinations
Regular comprehensive eye examinations can help detect any early signs of retinal tears or other retinal conditions. Early detection and prompt treatment can greatly improve the outcome.
Healthy Lifestyle Choices
Maintaining a healthy lifestyle can support overall eye health. This includes eating a balanced diet rich in fruits and vegetables, exercising regularly, maintaining a healthy weight, managing chronic conditions such as diabetes, and avoiding smoking.
Understanding and Managing Risk Factors
If you have certain risk factors, such as a family history of retinal detachment or a previous eye injury or surgery, it is important to discuss these with your ophthalmologist. They can provide guidance on proactive measures to minimize your risk of retinal detachment.
By understanding the causes, symptoms, treatment options, and preventive measures for retinal detachment, you can take proactive steps to preserve your vision. Remember, early detection and timely intervention are key to achieving the best possible outcomes. If you experience any warning signs or have concerns about your eye health, consult with an ophthalmologist for proper evaluation and management.